Disease Epidemiology/Clinical Course
Session: Poster Session A
(180) Utilizing Real World Data from a National Database of Living Donor Kidney Transplants to identify Targeted Subgroups for Planned Intervention Trials to prolong graft survival
Friday, August 25, 2023
8:00 AM - 6:00 PM ADT
Location: Convention Hall
Publication Number: 515
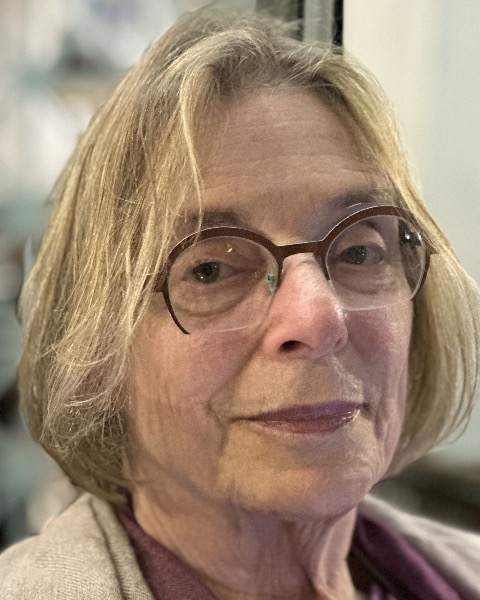
Joanna F. Haas, MD MSc FACP FACPM FISPE
Founding Partner
Haas and Partners LLC
Carlisle, United States
Presenting Author(s)
Background: Living donor kidney transplant (LDT) recipients have progressive renal function loss and graft failure, independent of graft rejection and immunosuppressive therapy
Objectives: Use of pretransplant factors to identify recipients at high risk of graft failure to improve efficiency of trials of novel interventions to prolong graft survival
Methods: The 2022 US Organ Procurement Transplant Network STAR data was accessed with permission. It includes complete information on all LDTs 1987-2022, including transplant date, patient descriptors, primary renal diagnosis, serology, organ preservation, surgery, followup, immunosuppressive therapy, graft and patient status, and cause of loss or death. Renal function by time was measured by creatinine and glomerular filtration rate (GFR). Outcome was death censored graft survival (DCGS), censoring deaths in patients with a functioning kidney. Graft survival was expressed as 75th Quartile (75Q) in yrs. Early renal function (ERF) was estimated as delayed graft function (dialysis in 1st week post transplant DGF), and GFR at discharge (GFRD). Predictor variables (PVs) for graft outcome were entered as categorical variables in Cox Proportional Hazard models and adjusted risk ratios and confidence limits estimated
Results: 168,609 patients received LDTs between 1987 and 2022 with 1,559,875 followup records. Following transplant, renal function progressively declined (GFR by 7% at 10 yrs)
A contemporary subset of 30,652 LDTs from 2010-2015 to allow adequate followup was analysed. Median recipient age 47 (18-89) donors 41 (11-84), median HLA mismatch 3 (0-6), 10% had 0 mismatch. DGF occurred in 3%. 8% died with functioning graft
DCGS was 22% at 10 yrs (75Q 11). 6 yr graft loss increased with decreasing recipient age from 5% to 18% , 75Q 16 to 6yr (RR 3.7; 3.3-4.2), increasing HLA mismatch (2.0; 1.7-2.4) and donor age (1.7; 1.5-1.8)
Both DGF and GFRD are PVs for DCGS. In the lowest GFRD decile 12% have graft loss before 3 yrs, but 2% for highest decile. The lower the GFR at discharge, the steeper the slope of graft loss. The major PVs of DGF are HLA mismatch, recipient and donor age
Conclusions: LDTs have progressive LRF, limiting graft survival. Identifying pretransplant risk factors for LRF and DCGS from RWD is the basis for designing strategies for new therapeutic intervention designs to prolong graft life in high risk subgroups. High risk includes young recipient age, older donor age and HLA mismatch. RWD from existing prospective unbiased data has utility to improve efficiency in clinical trial design by enriching target populations with those most likely to benefit, and forming a control group. Measuring ERF may have utility as an early efficacy signal in proof of concept trials and also provides a potential target for secondary prevention
Objectives: Use of pretransplant factors to identify recipients at high risk of graft failure to improve efficiency of trials of novel interventions to prolong graft survival
Methods: The 2022 US Organ Procurement Transplant Network STAR data was accessed with permission. It includes complete information on all LDTs 1987-2022, including transplant date, patient descriptors, primary renal diagnosis, serology, organ preservation, surgery, followup, immunosuppressive therapy, graft and patient status, and cause of loss or death. Renal function by time was measured by creatinine and glomerular filtration rate (GFR). Outcome was death censored graft survival (DCGS), censoring deaths in patients with a functioning kidney. Graft survival was expressed as 75th Quartile (75Q) in yrs. Early renal function (ERF) was estimated as delayed graft function (dialysis in 1st week post transplant DGF), and GFR at discharge (GFRD). Predictor variables (PVs) for graft outcome were entered as categorical variables in Cox Proportional Hazard models and adjusted risk ratios and confidence limits estimated
Results: 168,609 patients received LDTs between 1987 and 2022 with 1,559,875 followup records. Following transplant, renal function progressively declined (GFR by 7% at 10 yrs)
A contemporary subset of 30,652 LDTs from 2010-2015 to allow adequate followup was analysed. Median recipient age 47 (18-89) donors 41 (11-84), median HLA mismatch 3 (0-6), 10% had 0 mismatch. DGF occurred in 3%. 8% died with functioning graft
DCGS was 22% at 10 yrs (75Q 11). 6 yr graft loss increased with decreasing recipient age from 5% to 18% , 75Q 16 to 6yr (RR 3.7; 3.3-4.2), increasing HLA mismatch (2.0; 1.7-2.4) and donor age (1.7; 1.5-1.8)
Both DGF and GFRD are PVs for DCGS. In the lowest GFRD decile 12% have graft loss before 3 yrs, but 2% for highest decile. The lower the GFR at discharge, the steeper the slope of graft loss. The major PVs of DGF are HLA mismatch, recipient and donor age
Conclusions: LDTs have progressive LRF, limiting graft survival. Identifying pretransplant risk factors for LRF and DCGS from RWD is the basis for designing strategies for new therapeutic intervention designs to prolong graft life in high risk subgroups. High risk includes young recipient age, older donor age and HLA mismatch. RWD from existing prospective unbiased data has utility to improve efficiency in clinical trial design by enriching target populations with those most likely to benefit, and forming a control group. Measuring ERF may have utility as an early efficacy signal in proof of concept trials and also provides a potential target for secondary prevention

